Some children with speech sound disorders also have problems with their adenoids and tonsils. Sometimes, speech, adenoid and tonsil problems are related. Sometimes, they are not.
If your child has a chronically blocked nose, sleep apnea, otitis media with effusion and/or recurrent otitis media (middle ear infections), your child’s Ear Nose & Throat Specialist (ENT) may recommend removing her adenoids or tonsils (or both) (Brambilla et al, 2014). These are very common procedures, and can make a big difference to a child’s quality of life.
So how can adenoids and tonsils problems – and surgery to remove them – affect a child’s speech?
Here’s what the evidence tells us:
1. Why do we have adenoids and tonsils?
- The main purpose of adenoids and tonsils is to protect us from infection. They are placed to protect us from antigens from both the outside air (e.g. allergens and pathogens) and the alimentary tract (Brandtzaeg, 2003).
- Adenoids – also confusingly called pharyngeal tonsils (see diagram below) – are also important for the development of normal speech in children:
- They are located behind the soft palate behind the nose. Before puberty, when a child says an oral speech sound such as a vowel or voiced oral consonant (e.g. /d/, /l/, /g/ and /v/), the soft palate rises and touches the adenoids, creating a seal. This stops air from inappropriately coming up through the nose when speaking these sounds. The seal is essential for intelligible speech. (The soft palate lowers to allow air to come up through the nose when a child produces a nasal speech sound like /m/, /n/ and “ng”.)
- Adenoids become less important to speech with age. After puberty, at around 15 years of age, the adenoids shrink. At the same time, however, the wall at the back of the throat becomes more vertical. This means the soft palate can touch the back of the throat and maintain a good seal when producing vowels and oral voiced consonants.
- Tonsils – more precisely known as “palatine tonsils” – do not usually affect articulation or resonance.
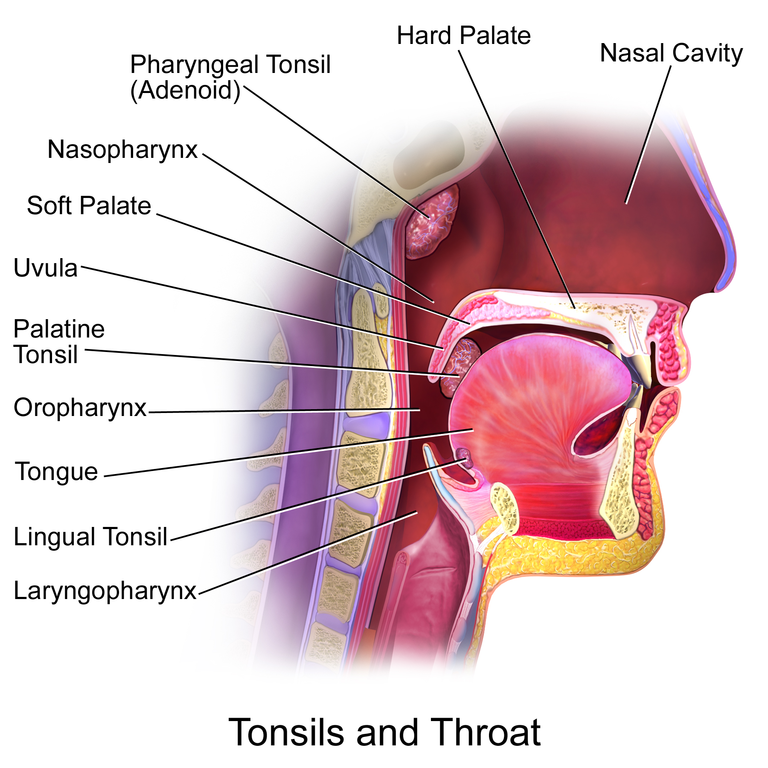 Image source: Blausen.com staff. “Blausen gallery 2014“. Wikiversity Journal of Medicine. DOI:10.15347/wjm/2014.010. ISSN 20018762. See: http://bit.ly/1nz4uxf
Image source: Blausen.com staff. “Blausen gallery 2014“. Wikiversity Journal of Medicine. DOI:10.15347/wjm/2014.010. ISSN 20018762. See: http://bit.ly/1nz4uxf
2. How can enlarged adenoids and their removal affect speech?
- Enlarged adenoids – “adenoid hypertrophy” – can be caused by recurrent or chronic respiratory infections. Several different conditions can lead to it, e.g. pollen and other allergies, passive smoking and viruses (e.g. the human adenovirus).
- Enlarged adenoids can cause:
- snoring, nasal obstruction, mouth breathing, recurrent sinusitis, auditory tube dysfunction, middle ear infections, reduced ability to smell and taste, changes in facial growth and behavioural development, and/or sleep apnea; and
- open mouth breathing and hyponasality – they may distort or prevent nasal speech sounds like /m/, /n/ and “ng”, and block nose breathing.
- The main cause of nasal obstruction for children is adenoid hypertrophy. But it’s important that an ENT be consulted, as it can also be caused by other conditions, e.g. rhinitis, nasal polyps, septel deviation and, on rare occasions, sino-nasal tumors. ENTs can conduct nasal endoscopies to investigate and diagnose the cause(s) of your child’s nasal congestion.
- In some cases, removing the adenoids can relieve hyponasality (blocked-nose resonance). However, sometimes the soft palate cannot establish a seal against the back of the throat immediately after the operation. This causes hypernasality, which is usually temporary.
- Hypernasality occurs when speech sounds are incorrectly transmitted through the nose, especially during the production of vowels and oral voiced consonants. For most children, this hypernasality reduces significantly within 3 months of the operation.
- In some cases, adenoid removal can have long-term negative effects on speech, especially if the child has a short soft palate, a large nasopharynx (the part of the pharynx behind and above the soft palate), a submucous cleft palate, or if their soft palate doesn’t work properly. Your child’s ENT should check these issues before recommending surgery.
- If hypernasality continues for more than 3 months after the adenoids are taken out, the child should be re-assessed by their ENT and referred to a speech-language pathologist.
3. How can enlarged tonsils and their removal affect speech?
- Enlarged tonsils can cause:
- hypernasality. Very large tonsils can “nestle” between the soft palate and the back of the throat causing a gap between both tonsils;
- a “potato-in-the-mouth” effect called “cul-de-sac resonance”, where air gets trapped in a blind pouch with only one exit; and
- a tongue fronting pattern where /k/, /g/ and “ng” are produced as /t/, /d/ and /n/ and, sometimes, a tongue thrust swallow. This is because the space usually occupied by the back of the tongue during production of “back” speech sounds is taken up by the enlarged tonsils, forcing the tongue to move forward (Shprintzen et al., 1987).
- Usually the hypernasality caused by enlarged tonsils is completely eliminated by the removal of the tonsils. Soft palate seal problems after tonsil removal are rare. But they can occur.
Clinical bottom line
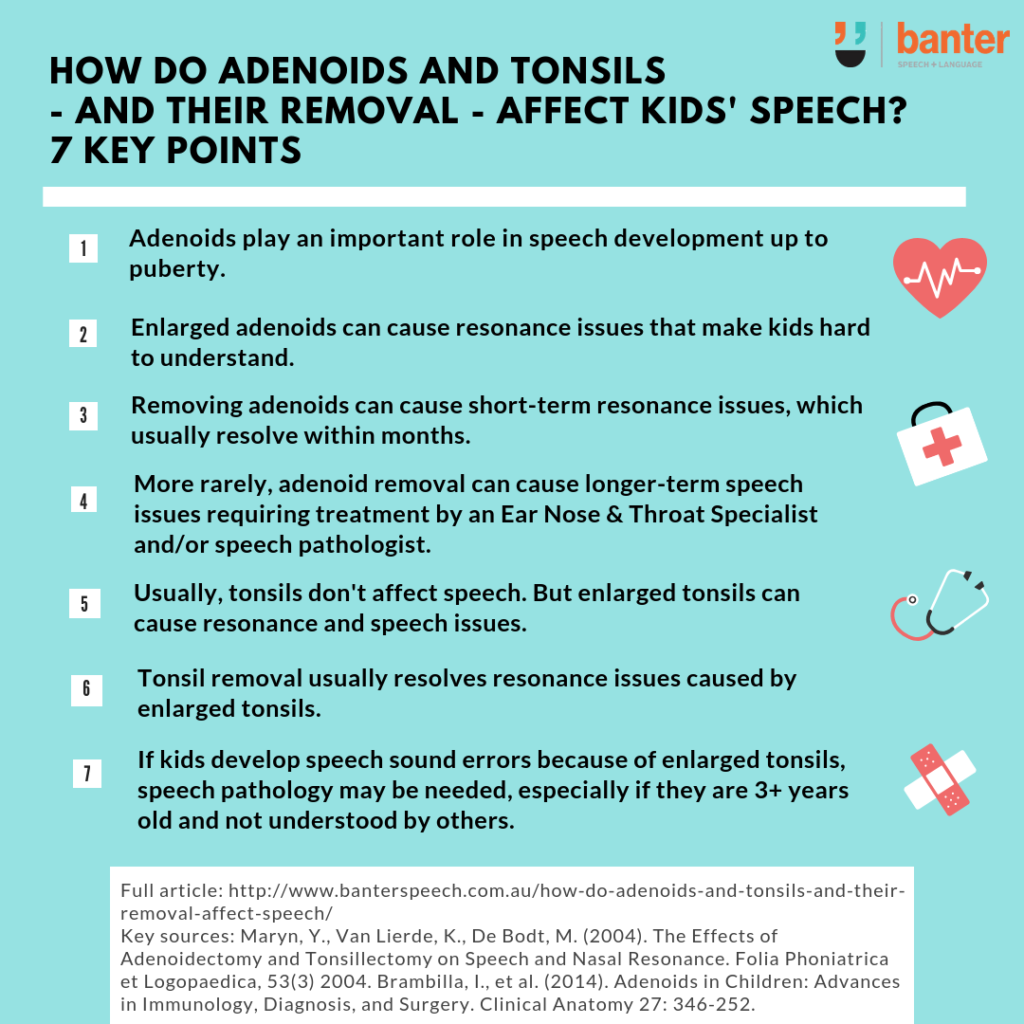
The adenoids play an important role in the speech development of children, at least up to puberty. Enlarged adenoids can cause resonance issues that affect a child’s intelligibility. Removing adenoids may cause short-term resonance issues, which usually resolve within a few months. More rarely, removal may cause longer term or permanent speech issues requiring further assessment and treatment by an ENT and/or speech pathologist.
Usually, the tonsils don’t affect speech or resonance. But enlarged tonsils can cause both resonance and speech issues. Removal of the tonsils usually resolves resonance issues caused by enlarged tonsils. But if your child has developed speech sound errors because of enlarged tonsils (e.g. fronting) which do not self-correct, a speech pathology assessment is recommended, especially if your child is older than 3 years and not intelligible to strangers.
Principal sources: Maryn, Y., Van Lierde, K., De Bodt, M. (2004). The Effects of Adenoidectomy and Tonsillectomy on Speech and Nasal Resonance. Folia Phoniatrica et Logopaedica, 53(3) 2004.
Brambilla, I., et al. (2014). Adenoids in Children: Advances in Immunology, Diagnosis, and Surgery. Clinical Anatomy 27: 346-252.
Related articles:
- “Stop talking through your nose!” What to do if you can’t help it
- FAQ: 10 common speech error patterns seen in children of 3-5 years of age – and when you should be concerned
Image: http://bit.ly/1NLA6oP

Hi there, I’m David Kinnane.
Principal Speech Pathologist, Banter Speech & Language
Our talented team of certified practising speech pathologists provide unhurried, personalised and evidence-based speech pathology care to children and adults in the Inner West of Sydney and beyond, both in our clinic and via telehealth.


What about production of the /r/ sound? Is it possible that enlarged tonsils and adenoids would prevent a child from pulling their tongue back enough to produce the /r/ sound?
Interesting question!
I’m not aware of any evidence of this and I would think it unlikely, especially if the underlying issue is phonological in nature (e.g. gliding of /r/ to /w/). I also don’t think tonsil/adenoid issues of themselves would affect retroflex tongue positions required for /r/, although again I’m not aware of any research about this. Thanks again for reading the article and your question.
Can enlarged tonsils affect the palatal growth due to restricted oxygen flow to the brain? My 9 year old suffers from an underbite and is currently undergoing an extensive othodontic treatment with palatal expanders, face mask, braces and eventual orthognathic surgery. We are having him evaluated this month for a tonsillectomy . I’m just anxious if this will work and resolve both underdeveloped palate as well as speech issues.
Hi – Thanks very much for your message. Unfortunately, we can’t answer questions like these because so much will depend on the specifics of your son’s situation, his health, and medical history, etc. To make a decision, you need specific professional advice tailored to your son’s needs. For this reason, we strongly encourage you to ask these questions of your son’s health team professionals, including his general practitioner, ENT, orthodontist, and speech pathologist. Sorry we can’t be of more direct help, and best of luck for your son!